Introduction
Physical therapy in Delray Beach for Hip Issues
Welcome to Miller PT's guide to hemiarthroplasty.
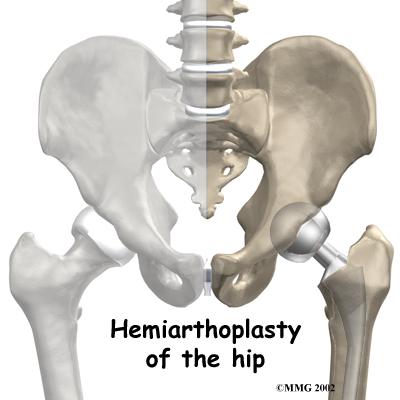
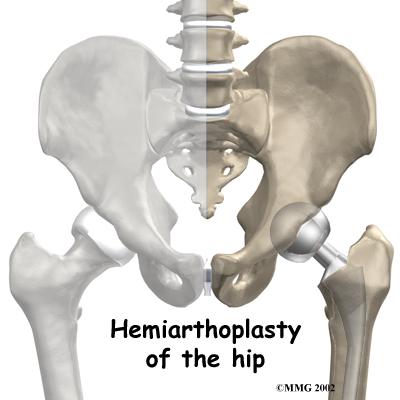
A hemiarthroplasty is an operation that is used most commonly to treat a fractured hip. The operation is similar to a total hip replacement but it involves only half of the hip. (Hemi means half, and arthroplasty means joint replacement.) The hemiarthroplasty replaces only the ball portion of the hip joint, not the socket portion. In a total hip replacement the socket is also replaced.
This guide will help you understand:
- what your surgeon hopes to achieve
- what happens during the operation
- what to expect after the procedure
- what Miller PT’s approach to rehabilitation is
Anatomy
How does the hip joint work?
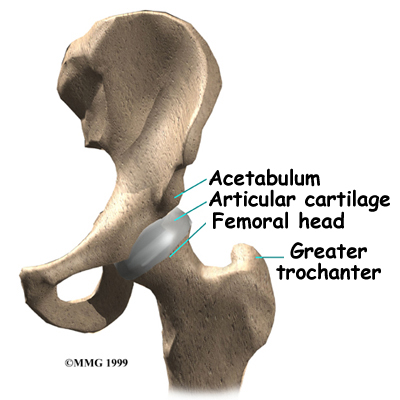 The hip joint is one of the true ball-and-socket joints of the body (the shoulder is the other.) The hip socket is called the acetabulum and forms a deep cup that surrounds the ball of the upper thighbone (femur,) known as the femoral head. The thick muscles of the buttock at the back, and the thick muscles of the thigh in the front surround the hip joint.
The hip joint is one of the true ball-and-socket joints of the body (the shoulder is the other.) The hip socket is called the acetabulum and forms a deep cup that surrounds the ball of the upper thighbone (femur,) known as the femoral head. The thick muscles of the buttock at the back, and the thick muscles of the thigh in the front surround the hip joint.
The surface of the femoral head and the inside of the acetabulum are covered with articular cartilage. This material is about one-quarter of an inch thick in most large joints. Articular cartilage is a tough, slick material that allows the joint surfaces to glide against one another without damage.
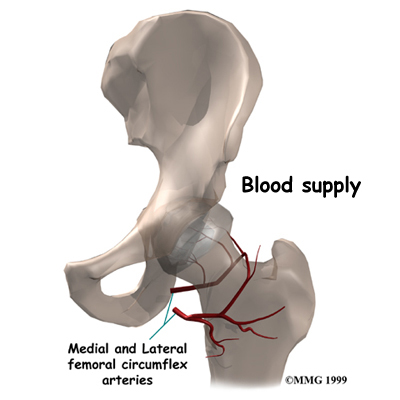
All of the blood supply to the femoral head (the ball portion of the hip) comes through the neck of the femur (femoral neck), which is a thinner section of the thighbone that connects the ball to the main shaft of the bone.If this blood supply is damaged, there is no backup.
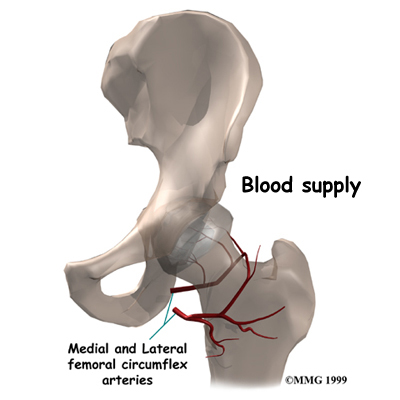
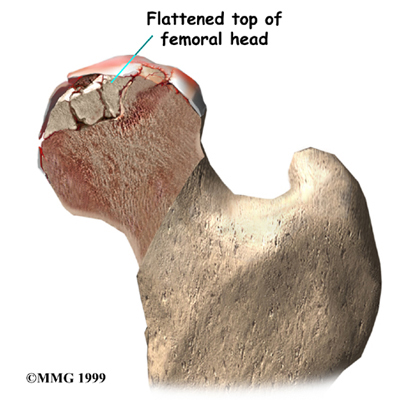
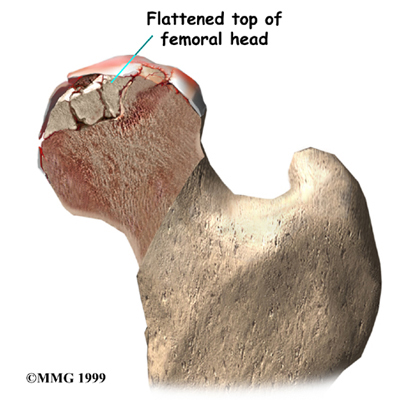
One of the problems with hip fractures is that damage can occur to these blood vessels when the hip breaks and this damage can lead to the bone of the femoral head actually dying. This dying of the bone, called avascular necrosis (AVN), is always a potential complication of a hip fracture. The problem with leaving dead bone in the hip is that it may eventually collapse, causing pain in the hip, and decreased hip function.
Related Document: Miller PT's Guide to Avascular Necrosis of the Hip.
Related Document: Miller PT's Guide to Hip Anatomy.
Rationale
What do surgeons hope to achieve with the operation?
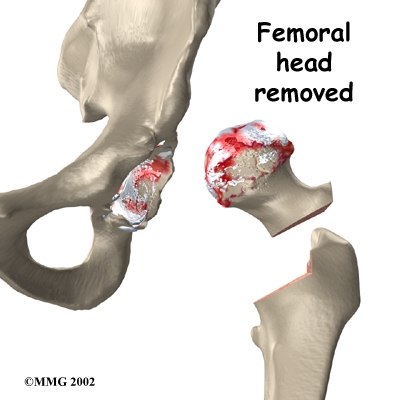
Fractures of the hip often involve the femoral neck. In many cases, the risk of developing AVN is so high that your surgeon may suggest not fixing the fracture because by fixing it there is still a high chance that you will need a second operation several months later if the femoral head dies due to AVN. Instead, it is often recommended that the femoral head be removed and replaced with an artificial piece, or prosthesis.
When the hip is fractured, the socket portion (the acetabulum) is usually not injured. If the articular cartilage of the hip socket is in good condition, the metal ball of the hemiarthroplasty prosthesis can glide against the cartilage without damaging the surface. A hemiarthroplasty is easier to do than replacing both the ball and the socket (a total hip replacement), and it allows patients to move better and quicker after surgery. Early movement is particularly important in the elderly population as it helps prevent dangerous, and possibly life-threatening complications that come from being immobilized in bed, and also lets patients more quickly return to independent function.
Related Document: Miller PT's Guide to Hip Fractures.
Preparations
How should I prepare for surgery?
This procedure is usually an emergency surgery so it is likely you will not have had time to plan and prepare. Ideally, a caregiver, such as a family member or friend, will help make arrangements for you while you are in the hospital. The surgeon and care team will communicate with your caregiver to help with these preparations. Your caregiver will help coordinate your ride home, prepare your home for your arrival, obtain any needed supplies, and schedule follow-up appointments with your surgeon, general practitioner, and physical therapist.
Surgical Procedure
What happens during the operation?
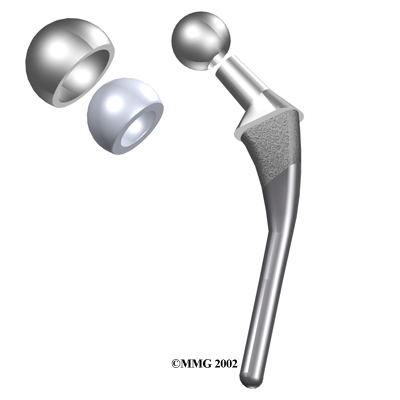
As described earlier, the hemiarthroplasty prosthesis replaces the femoral head. The prosthesis is composed of a metal stem that fits into the hollow marrow space of the thighbone (the femur). It also has a metal ball that fits into the socket of the hip joint (the acetabulum).
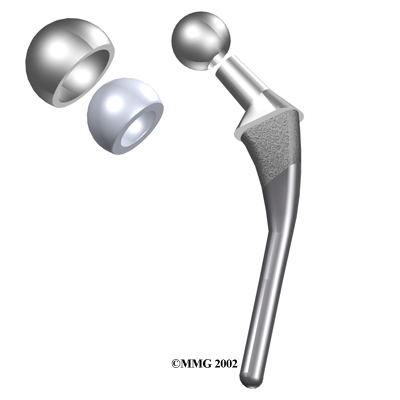
The femoral head that attaches to the stem may be a separate part. Two types are commonly used by surgeons. Some surgeons prefer a solid metal ball to replace the femoral head. This type of prosthesis is called a unipolar type. Other surgeons prefer to use a bipolar type of prosthesis. The bipolar type has a femoral head that swivels where it attaches to the stem. The bipolar prosthesis was designed to try to reduce the wear and tear on the articular cartilage inside the acetabulum. It is unclear whether the swivel offers any significant advantages; both types seem to work well.
A cemented prosthesis is held in place by a type of epoxy cement that attaches the metal to the bone. An uncemented prosthesis bears a fine mesh of holes on the surface that allows bone to grow into the mesh and attach the prosthesis to the bone. Both methods are still widely used. The decision about whether to use a cemented or uncemented prosthesis is made by each surgeon based on your age, the condition of your bones, your lifestyle, and the surgeon's experience.
The Operation
To begin, the surgeon makes an incision to allow access to the hip joint. Different approaches can be used to make the incision. Sometimes the incision is made posterior to the joint and sometimes it is made anterior to the joint. The choice of surgical approach is usually based on the surgeon's training and preferences.
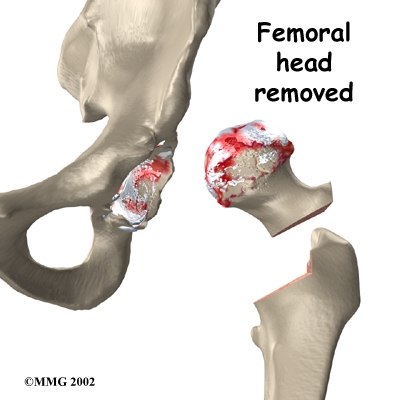
Once the hip joint is entered, the surgeon removes the femoral head from the acetabulum.
Special rasps (coarse files) are used to shape the hollow femur to the exact shape of the metal stem of the prosthesis. Once the size and shape are satisfactory, the stem is inserted into the femoral canal. Again, in the uncemented version the stem is held in place by the tightness of the fit into the bone (similar to the friction that holds a nail driven into a hole slightly smaller than the diameter of the nail). In the cemented variety, the femoral canal is enlarged to a size slightly larger than the femoral stem, and an epoxy-type cement is used to bond the metal stem to the bone. The metal ball that makes up the femoral head is then attached.
Once the implant is in place, the new artificial hip is put back into the hip socket (also called relocating or reducing the hip). The surgeon makes sure that the hip works properly and the joint moves easily. The surgeon then closes the incision with several layers of stitches under the skin and uses stitches or metal staples to close the skin itself. A large bandage is placed over the incision and special boots and/or compression type stockings, which help to move the fluid in your legs, are placed on your lower legs and feet to assist in preventing the formation of blood clots. A triangle-shaped cushion may be positioned between your legs to keep your legs from crossing or rolling in. You are then returned to the recovery room.
After Surgery
What happens after surgery?
Due to the use of anesthesia and the associated immobility that occurs with a surgery, all surgical patients are at risk of developing pneumonia. For this reason, once you are awake you will be instructed immediately to begin deep breathing exercises. You may even be given an incentive spirometer to encourage deep breathing. An incentive spirometer is a small handheld device that allows you to visually see a small ball rise in response to taking a deep breath. At least ten deep breaths should be taken each hour, particularly while you are not moving much. As you begin to move around more, you will naturally take deep breaths so it is not as crucial to remember to do them each hour. It is interesting to note that laughing and yawning are natural ways to take in deep breaths as well! In addition to deep breathing exercises you will be instructed to pump your ankles up and down and do ankle circles to encourage movement of the fluid in your legs in order to avoid a deep vein thrombosis (DVT), more commonly known as a blood clot.
Inpatient physical therapy will be scheduled at least once a day as long as you are in the hospital. Usually your first visit from the physiotherapist will be soon after you are settled into your room. Your therapist will review the deep breathing and ankle pumping exercises and will also instruct you on how to get the muscles of your buttocks and thigh activated by tightening them without moving the hip or knee joints.
Your physical therapist will also review the movements that you must avoid doing to protect your hemiarthroplasty (also called the hip precautions). These movements are dangerous as they can cause your hip to dislocate. The risk of dislocation is greatest right after surgery. Once the tissues around the hip heal and you have built up the strength of the muscles surrounding the hip, the risk significantly decreases. The movements most likely to cause dislocation of your hip depend on which approach to surgery, anterior or posterior, that your surgeon used. If an anterior approach was used, then extending the hip back, turning your hip and leg out, or spreading your leg outwards should be avoided. If your surgeon used a posterior approach, then crossing your legs, turning your hip and leg inward, or bending the hip more than 90 degrees are the motions that should be avoided. Your therapist will educate you on the precautionary movements pertaining to your particular surgery.
How quickly you start getting up from the bed depends on your surgeon’s protocol. Some surgeons request that you get up from your hospital bed and move to a chair on the day of your surgery. Others wait until the day after your surgery. Even this small activity of moving from your bed to a chair is extremely beneficial to your recovery from surgery, as it helps to get the fluid in your legs moving, activate your muscles, and encourage deep breathing.
By the second session, your therapist will instruct you on more advanced exercises where you are moving your hip and knee to both encourage range of motion as well as to start to strengthening your muscles. In addition to more advanced exercises, you will begin to walk short distances with either a walker or crutches. Most patients are allowed to put as much weight as is comfortable down through their foot when standing or walking. If, however, your surgeon used a non-cemented prosthesis you may be instructed to limit the weight you put on your foot. Your therapist will clarify for you how much weight is allowed in your particular situation.
The majority of patients begin walking using a walker, and progress to crutches if they are able, and if they have stairs to negotiate at home. Crutches allow you to be much more mobile, but they do require more coordination. If you are not steady on the crutches, even with practice, a walker is recommended even for when you go home. The walker, however, cannot be used on typical stairs. Most patients progress to using a cane (in the hand opposite to their surgical leg) in three to four weeks. Once you can walk without a limp and your muscles are strong enough, no walking aid is used. Generally this is around the 6-week mark, but can be earlier, or may be later, depending on your ability, as well as your surgeon’s restrictions.
Each day after surgery you will be expected to independently complete your exercises and go for a walk. A therapist will visit you on most, if not all days, to ensure that you are progressing well and that you are learning to do your rehabilitation program independently. If your hospital has a pool, and your surgeon allows it, hydrotherapy may be incorporated once your surgical incision stops oozing. The buoyancy, hydrostatic properties, and warmth of the water often allow easier and less painful hip movements.
In addition to providing you with a rehabilitation program, your physical therapist or an occupational therapist will discuss recommendations for home modifications that will allow you to abide by the hip precautions and create a safe environment. These recommendations may include using a raised commode seat, using a bathtub bench, and raising the surfaces of couches and chairs to keep your hip from bending too far when you sit down. Bath benches and handrails can greatly improve safety in your bathroom and are highly recommended. Other suggestions may include the use of strategic lighting and the removal of loose rugs or electrical cords from the floor in order to avoid tripping or falling.
Patients can usually be discharged home after spending anywhere from three to ten days in the hospital. Factors that determine how long you will remain in the hospital are: Your surgeon’s protocol, your ability to independently get in and out of bed, your ability to properly perform your rehabilitation exercises, your ability to walk safely for a moderate distance with your crutches or walker, your ability to safely use crutches to go up and down stairs (if you have stairs at home), and your ability to consistently remember to use your hip precautions. Patients who still need extra rehabilitation care after they are medically stable in the hospital may be sent to a different hospital unit until they are independently safe to go home. Alternatively, they may go home if they have adequate family support and a physical therapist can visit them at their home until they are able to demonstrate the above skills. Not all patients, however, will require physical therapy in their own home.
Your staples will be removed 10-14 days after surgery. Patients are usually able to drive within three weeks. Upon the approval of the physician, patients are generally able to resume sexual activity one to two months after surgery.
Miller PT provides services for physical therapy in Delray Beach.
Rehabilitation
What should I expect during my rehabilitation after leaving the hospital?
After you are discharged from the hospital, you should continue your home rehabilitation program. If needed, a therapist may see you in your home for a few treatments, but this is generally only until you are able to safely get out of your home. Once you are independent enough to attend physical therapy outside of the home, even if someone else needs to drive you, you should begin treatment at Miller PT to continue your rehabilitation. The most important part of your rehabilitation after a hip hemiarthroplasty will be the exercises that you do independently at home, however, by attending Miller PT for physical therapy we will be able to ensure that you are doing your exercises well, ensure you are doing the correct exercises for your level of healing, advance your exercises as you improve, and ensure that there are no factors in your individual case that will impede your recover or your return to function.
If you are still using a walker or crutches by the time we first see you at Miller PT, your physical therapist will ensure you are using them safely, properly, and confidently while abiding by your weight bearing restrictions. We will also ensure that you can safely use crutches on stairs. If you are no longer using a walking aid, or once you no longer need one, your physical therapist will focus on normal gait re-education so you are putting only the necessary forces through the surgical side with each step, and are not compensating in any way. Until you are able to walk without a significant limp, we recommend that you continue to use a walking aid, such as your crutches, or a cane/stick. Improper gait can lead to a host of other pains in the knee, hip and back so it is prudent to use a walking aid until virtually normal walking can be achieved. Your Miller PT physical therapist will advise you regarding the appropriate time for you to be walking without any walking aid at all.
As mentioned above, a hip hemiarthroplasty is at risk of dislocating if it is forced into certain motions, so the hip precautions you have been taught must be strictly respected, particularly in the early stages after surgery, until the incision heals and strength is regained in the muscles around the hip and in the leg. At your first appointment your physical therapist will again discuss the hip precautions pertaining to your surgical procedure. The length of time that hip precautions should be abided by varies in opinion. Many surgeons suggest 12 weeks, however, other surgeons or health care professionals recommend much longer, even up to 1-2 years or forever, if possible! How long you must abide by your hip precautions depends on a number of factors. Certainly 12 weeks minimum is a must. Other factors affecting the length of time include: your surgeon’s protocol and recommendation based on your specific case, your muscle strength, your muscular control of the hip, your risk of falling, if you are obese, if you are very thin with little muscular support, and how active or inactive you are or want to be. Your physical therapist at Miller PT will be able to discuss your individual situation regarding hip precautions.
During your first few appointments at Miller PT your physical therapist will focus on relieving any pain and/or inflammation you may still have from the surgical procedure. They may use modalities such as ice, heat, ultrasound, or electrical current to assist with decreasing any pain or swelling you have around the surgical site or anywhere down the extremity. In addition, your physical therapist may massage your hip, back, leg or ankle to improve circulation and help decrease your pain.
The next part of our treatment will focus on regaining the range of motion in your hip. Your physical therapist at Miller PT will prescribe a series of stretching exercises that you will practice in the clinic and also add to your home exercise program. Some of these exercises may be similar to the exercises that you learned in the hospital and that you have already been doing at home. Many of the home exercises will have become too simple for you by this stage of your rehabilitation so your therapist will ensure that you are doing the most advanced exercises for your stage of recovery in order to ensure you progress as quickly as possible. Hip precautions will need to be strictly abided by in all of your exercises so it is best not to add any exercises into your program independently, but rather to allow your therapist to shape your individual program as they see fit for your current ability.
Range of motion in the hip generally comes back very quickly after a hemiarthoplasty. You may experience a small amount of discomfort at the end ranges of motion initially, but despite this it is important to perform the range of motion exercises as prescribed because moving the joint also helps to diminish the swelling, get fresh blood to the healing areas, and provides nutrition to the joint. Only mild discomfort, however, is permissible. Any sharp or moderate discomfort should be heeded. An exercise bike at this stage of recovery can be very useful, however you must still respect your hip precautions while using the bike, therefore the advice of your therapist regarding bike set up is crucial the first few times you attempt it.
If necessary, and as time and healing allows, your physical therapist may mobilize your hip joint. This hands-on technique encourages the hip to move gradually into its normal range of motion. Mobilization of the hip may be combined with assisted stretching of any tight muscles around the surgical site.
Your therapist will also review and advance your strengthening exercises. Again, as you progress you will outgrow the strengthening exercises that were given to you in the hospital so it is important that your physical therapist at Miller PT advances your exercises to suit your level of progress. These exercises will focus on the muscles of your hip and thigh but will also include some exercises for your back and core area as they play a large supporting role for your hips. Exercises that involve the entire lower limb, such as squats (on both legs at the same time or just one leg,) will also be given.
Exercises that work the muscles while in standing most effectively assist with daily activities such as walking and stair climbing. Other exercises in sitting or lying, however may also be prescribed. Exercises in these positions can be excellent in allowing you to target specific muscles around the hip, such as the gluteals, without causing you any discomfort from too much body weight being on the hip. Your therapist may use an electrical muscle stimulator to assist your muscles in contracting as you do your exercises; this will help you to more rapidly gain your strength back. Exercises may also include the use of exercise bands or weights to provide some added resistance for your hip and lower extremity. If you have access to a pool, your therapist may suggest you go to the pool to do your exercises. As mentioned above, the buoyancy and hydrostatic properties of the water along with the warmth of the water (provided it is a heated pool) can assist greatly in providing comfort to the hip joint and often allows your exercises to be done more easily and with less discomfort.
As a result of any injury or surgery, the receptors in your joints and ligaments that assist with balance and proprioception (the ability to know where your body is without looking at it) decline in function. A period of immobility and reduced weight bearing will add to this decline. When balance and proprioception is diminished, your joints and your limb as a whole will not function as efficiently and the decline may contribute to further injury in the future. Once you are able to put full weight onto your surgical side a final component of our treatment at Miller PT will be to prescribe exercises for you to regain this balance and proprioception. These exercises might include activities such as standing on one foot or balancing on an unstable surface such as a soft mat, or a soft plastic disc.
Proprioceptive exercises are important for all patients who have had surgery but they are particularly important for patients who have had a hip hemiarthroplasty because often the reason for the surgery was due to a fracture of the hip resulting from a fall. By improving one’s proprioception, you can decrease your chances of another fall, which may result in damage to your surgical hip, or worse yet, a fracture of the other hip or another bone in your body.
During all of your exercises your physical therapist at Miller PT will pay particular attention to your exercise technique to ensure that you are not using any compensatory patterns or are developing bad habits in regards to how you use your hip and lower extremity. If you do not pay close attention to how you use your joint and limb post-surgically inefficient patterns can quickly occur and compensatory pain will develop either in your hip, back, or another joint. The acetabulum of the hip can also begin to quickly wear down, leading to the need for it to also be replaced, if your exercise technique or walking pattern is not pristine. Your physical therapist at Miller PT will be crucial for providing you with feedback regarding correcting these patterns and developing new, efficient patterns during your daily activities.
As your range of motion, strength, and proprioception improve, your therapist will advance your exercises to ensure your rehabilitation is progressing as quickly as your body allows, and to incorporate exercises that simulate your specific everyday activities of daily living and any recreational activities that you may want to return to. Many patients undergoing this surgery are older, and are not still regularly active. However, there are also younger patients for whom this surgery is required. For these younger patients unfortunately, heavy sports that require running, jumping, quick stopping and starting, and cutting are discouraged. Patients may also need to consider alternate jobs to avoid work activities that require heavy demands of lifting, crawling, and climbing. Your surgeon will advise you which activities in your case are not at all permissible or are discouraged.
Your physical therapist at Miller PT’s goal is to help you maximize range of motion, strength and proprioception, as well as walk normally, and improve your ability to do your activities. When you are well under way, regular visits to our clinic will end. Your physical therapist will continue to be a resource, but you will be in charge of doing your exercises as part of an ongoing home program.
Generally the rehabilitation after a hemiarthroplasty responds very well to the physical therapy we provide at Miller PT. If for some reason, however, your pain continues longer than it should or your therapy is not progressing as your physical therapist would expect, we will ask you to follow-up with your surgeon to confirm that the hip is tolerating the rehabilitation well and ensure that there are no complications that may be impeding your recovery.
Miller PT provides services for physical therapy in Delray Beach.
Complications
What might go wrong?
As with all major surgical procedures, complications can occur. A few of the potential complications have already been touched on in the information above, but are discussed in further detail below. The following is not a complete list of the possible complications, but rather some of the most common problems, which include:
- anesthesia complications
- thrombophlebitis
- infection
- dislocation
- loosening
- ongoing pain
Anesthesia Complications
Most surgical procedures require that some type of anesthesia be used before surgery. A very small number of patients have problems with anesthesia such as a reaction to the drugs used, or a problem under anesthesia related to other medical complications. Be sure to discuss the risks and your concerns with your anesthesiologist.
Thrombophlebitis (Blood Clots)
Thrombophlebitis, sometimes called a deep venous thrombosis (DVT), can occur after any operation, but is more likely to occur following surgery on the hip, pelvis, or knee. DVT occurs when blood clots form in the large veins of the leg. These clots may cause the leg to swell and become warm to the touch and painful. Even more dangerously, if the blood clots in the veins break apart, they can travel to the lungs where they lodge in the capillaries and cut off the blood supply to a portion of the lung. This is called a pulmonary embolism. (Pulmonary means lung, and embolism refers to a fragment of something traveling through the vascular system.) Surgeons take preventing DVT very seriously. There are many ways to reduce the risk of DVT, but one of the most effective ways is to get you moving as soon as possible after surgery. Two other commonly used preventative measures include:
- pressure stockings or pumps to keep the blood in the legs moving
- medications that thin the blood and prevent blood clots from forming
Infection
Infection in any surgery, such as a hip hemiarthroplasty, can be a very serious complication. The chance of getting an infection following hemiarthroplasty is approximately one percent. Some infections may show up very early, even before you leave the hospital. Others may not become apparent for months, or even years, after the operation. Infection can spread into the artificial joint from other infected areas. To reduce the risk of spreading germs to your joint your surgeon may ask you to take antibiotics when you have dental work or surgical procedures on your bladder or colon.
Dislocation
By opening up your hip joint to perform the hemiarthroplasty, your surgeon must cut through the soft tissues around your hip (the joint capsule and ligaments), which normally provide stabilization to your joint. Due to this, your hip after surgery is at risk of dislocating (the ball coming out of the socket.) There is a greater risk of dislocation immediately after surgery, before the tissues have healed around the joint, but there is always a risk. Your physical therapist will instruct you on which activities and positions to avoid that may have a tendency to cause a hip dislocation. A hip that dislocates more than once may have to be revised with another surgery to make it more stable. Patients with diseases such as Parkinson's or Alzheimer's are at a higher risk of dislocating their hip. With Parkinson’s this risk is increased due to the uncontrollable associated movements of the disease and higher risk of falling. In patients with Alzheimer’s, the inability to consistently follow the hip precautions increases their risk of dislocation.
Related Document: Miller PT's Guide to Artificial Hip Dislocation Precautions
Loosening
The main reason that joint implants eventually fail continues to be loosening of the metal or cement from the bone. Great advances have been made in extending how long artificial replacement parts will last, but most will eventually loosen and require a revision.
Generally you can expect 12 to 15 years of service from replacement parts for the hip, but in some cases the hip will loosen earlier than that. A loose hip is a problem because it causes pain and affects the biomechanics of the joint, which then causes further wear and tear on the joint itself as well as other associated joints. Once the pain becomes unbearable, another operation is often required to revise the hip.
Ongoing Pain
A hemiarthroplasty replaces the ball portion of the hip joint, but does not replace the socket of the joint. This means that the metal ball is constantly rubbing against the articular cartilage that lines the inside of your natural hip socket. The socket may become arthritic as the cartilage wears out over time. If this occurs, the hip will become painful just like any other arthritic joint. If the pain becomes unbearable, the hemiarthroplasty may need to be converted to a completely artificial joint. This means that the socket will be replaced with a new artificial socket. Fortunately the metal stem does not always need to be replaced when this occurs.
Most orthopedic surgeons recommend that you have routine checkups after undergoing a hip hemiarthroplasty. How often you need to be seen varies from every six months to every five years, according to your individual situation and what your surgeon recommends. Obviously, if at any time post surgically you feel like your hip suddenly declines in function or you are experiencing more pain that usual, a follow up with your surgeon would be prudent.
Portions of this document copyright MMG, LLC.







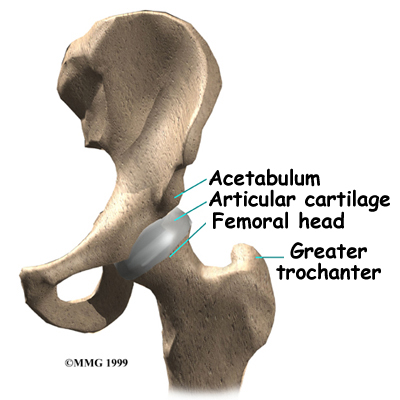 The hip joint is one of the true ball-and-socket joints of the body (the shoulder is the other.) The hip socket is called the acetabulum and forms a deep cup that surrounds the ball of the upper thighbone (femur,) known as the femoral head. The thick muscles of the buttock at the back, and the thick muscles of the thigh in the front surround the hip joint.
The hip joint is one of the true ball-and-socket joints of the body (the shoulder is the other.) The hip socket is called the acetabulum and forms a deep cup that surrounds the ball of the upper thighbone (femur,) known as the femoral head. The thick muscles of the buttock at the back, and the thick muscles of the thigh in the front surround the hip joint.