Introduction
Physical therapy in Delray Beach for Hand
Welcome to Miller PT's patient resource about Guyon's Canal Syndrome.
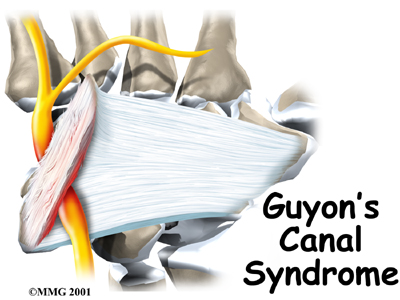
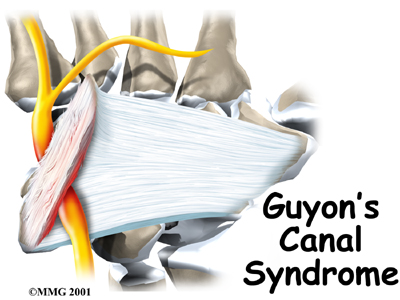
Guyon's canal syndrome is an entrapment of the ulnar nerve as it passes through a tunnel in the wrist called Guyon's canal. This problem is similar to carpal tunnel syndrome but involves a completely different nerve. Sometimes both conditions can cause a problem in the same hand.
This guide will help you understand:
- how Guyon's canal syndrome develops
- how doctors diagnose the condition
- what can be done to treat the problem
Anatomy
Where is the ulnar nerve, and what does it do?
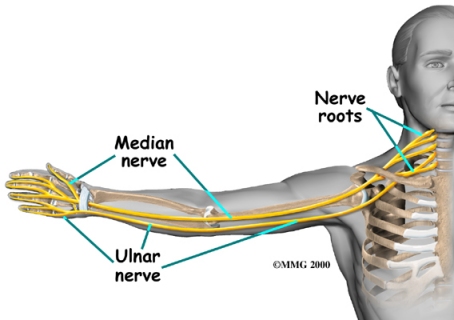
The ulnar nerve actually starts at the side of the neck, where the individual nerve roots exit the spine through small openings between the vertebrae. The then join together to form three main nerves that travel down the arm to the hand, one of which is the ulnar nerve.
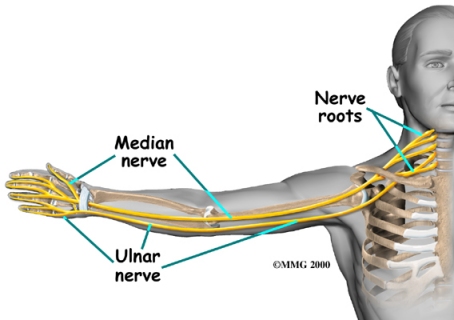
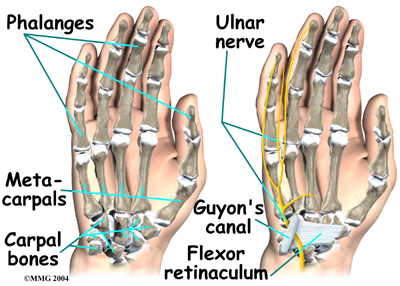
After leaving the side of the neck, the ulnar nerve travels through the armpit and down the arm to the hand and fingers. As it crosses the wrist, the ulnar nerve and ulnar artery run through the tunnel known as .
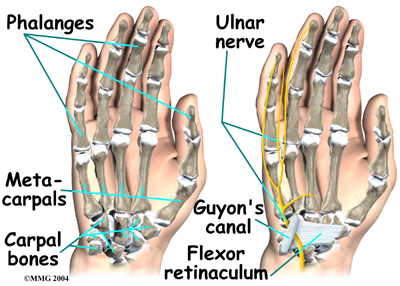
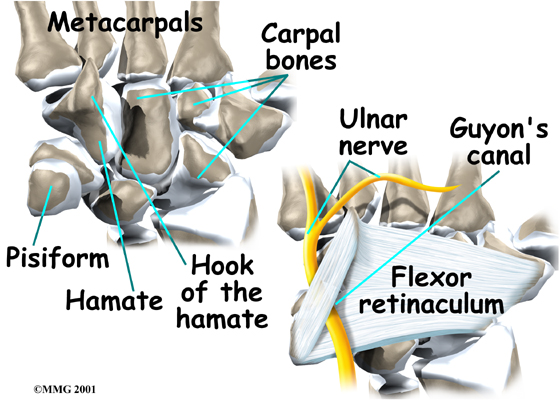
This tunnel is (the pisiform and hamate) and the ligament that connects them. After passing through the canal, the ulnar nerve branches out to supply feeling to the little finger and half the ring finger. Branches of this nerve also supply the small muscles in the palm and the muscle that pulls the thumb toward the palm.
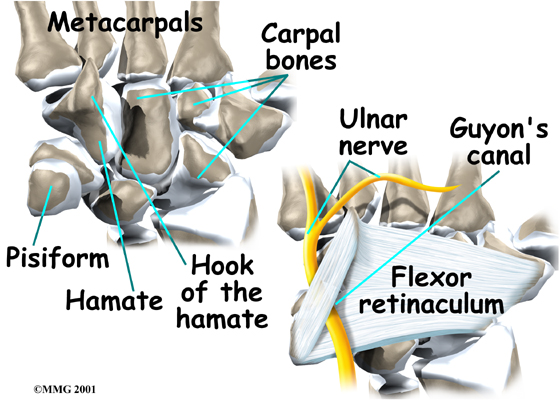
The hamate bone forms one side of Guyon's canal. This bone has a small hook-shaped spur that sticks out to provide an attachment for several wrist ligaments. Known as the hook of hamate, this small bone can break off and press against the ulnar nerve within Guyon's canal.
Related Document: Miller PT's Guide to Hand Anatomy
Hand Anatomy Introduction
Causes
Why do I have this problem?
 Guyon's canal syndrome has several causes. Overuse of the wrist from heavy gripping, twisting, and repeated wrist and hand motions can cause symptoms. Working with the hand bent down and outward can squeeze the nerve inside Guyon's canal.
Guyon's canal syndrome has several causes. Overuse of the wrist from heavy gripping, twisting, and repeated wrist and hand motions can cause symptoms. Working with the hand bent down and outward can squeeze the nerve inside Guyon's canal.
Constant pressure on the palm of the hand can produce symptoms. This is common in cyclists and weight lifters from the pressure of gripping. It can also happen after running a jackhammer or when using crutches.
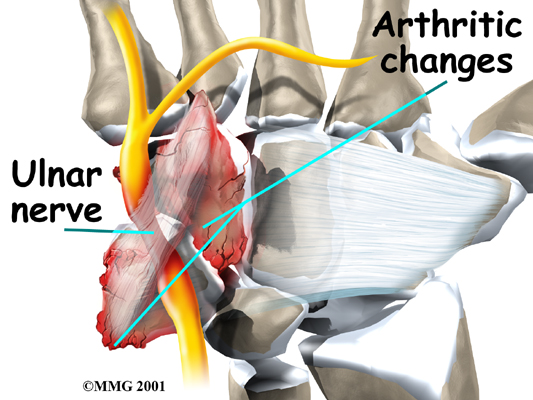
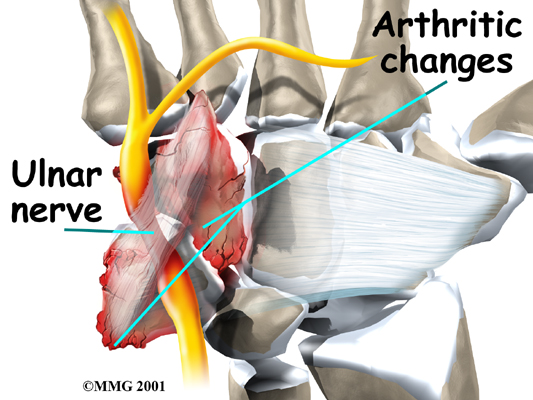
Pressure or irritation of the ulnar nerve can cause symptoms of Guyon's canal syndrome. A traumatic wrist injury may cause swelling and extra pressure on the ulnar nerve within the canal. and joints may eventually irritate and compress the ulnar nerve. In rare cases, the ulnar artery that travels right beside the nerve may be damaged and form a blood clot. The symptoms caused by the clot mimic Guyon's canal syndrome. The lack of blood supply to the ulnar nerve is believed to cause the symptoms.
As mentioned earlier, a in the wrist can pinch the nerve inside Guyon's canal. This bone is sometimes fractured when golfers club the ground instead of the golf ball and when baseball players are batting.
Symptoms
What does Guyon's canal syndrome feel like?
Symptoms usually begin with a feeling of pins and needles in the ring and little fingers, which is often noticed in the early morning when first awakening. This may progress to a burning pain in the wrist and hand followed by decreased sensation in the ring and little fingers. The hand may become clumsy when the muscles controlled by the ulnar nerve become weak. Weakness can affect the small muscles in the palm of the hand and the muscle that pulls the thumb into the palm. Gradual weakness in these muscles makes it hard to spread your fingers and pinch with your thumb.
This syndrome is much less common than carpal tunnel syndrome (CTS), yet both conditions can occur at the same time. The numbness caused by these two syndromes affects the hand in different locations. When the median nerve is compressed in CTS, pain and numbness spread into the thumb, index finger, middle finger, and half of the ring finger. Compression of the ulnar nerve in Guyon's canal syndrome usually causes numbness in the pinky and half of the ring finger.
Related Document: Miller PT's Guide to Carpal Tunnel Syndrome
Diagnosis
When you visit Miller PT, diagnosis of Guyon's canal syndrome begins with a careful history and physical examination by our physical therapist. Compression can occur at several areas along the ulnar nerve, and we will test to find exactly where the nerve is being affected.
Some patients may be referred to a doctor for further diagnosis. Once your diagnostic examination is complete, the physical therapists at Miller PT have treatment options that will help speed your recovery, so that you can more quickly return to your active lifestyle.
Our Treatment
Non-surgical Rehabilitation
When you begin your physical therapy program, our physical therapist will recommend that you change or stop the activities that might be causing your symptoms if at all possible. Avoid repetitive hand motions, heavy grasping, resting your palm against hard surfaces, and positioning or working with your wrist bent down and out.
 We may have you wear a in the early stages of Guyon's canal syndrome. A brace keeps the wrist in a resting position (neither bent back nor bent down too far). It can be especially helpful for easing the numbness and pain felt at night because it can keep your hand from curling under as you sleep. The wrist brace can also be worn during the day to calm symptoms and rest the tissues within the canal.
We may have you wear a in the early stages of Guyon's canal syndrome. A brace keeps the wrist in a resting position (neither bent back nor bent down too far). It can be especially helpful for easing the numbness and pain felt at night because it can keep your hand from curling under as you sleep. The wrist brace can also be worn during the day to calm symptoms and rest the tissues within the canal.
We may also recommend anti-inflammatory medications. Common over-the-counter medications, such as ibuprofen and aspirin, can also help control the symptoms of Guyon's canal syndrome.
The main focus of your Miller PT treatment is to reduce or eliminate the cause of pressure on the ulnar nerve. Our physical therapist may check your workstation and the way you do your work tasks. We will provide suggestions about the use of healthy body alignment and wrist positions, helpful exercises, and tips on how to prevent future problems.
Although the rate of recovery is different for each patient, if nonsurgical treatment is successful, you may see improvement in four to six weeks. We may recommend that you continue wearing your wrist splint at night to control symptoms and keep your wrist from curling under as you sleep. Try to do your activities using healthy body and wrist alignment. Limit activities that require repeated motions, heavy grasping, and pressure on the palm of the hand.
Post-surgical Rehabilitation
 Your hand will be wrapped in a following surgery. When you begin your recovery, our physical therapist will advise you to take time during the day to support your arm with your hand elevated above the level of your heart. We will encourage you to move your fingers and thumb occasionally during the day. Keep the dressing on your hand until you return to the surgeon. Avoid getting the stitches wet. Your stitches will probably be removed 10 to 14 days after surgery.
Your hand will be wrapped in a following surgery. When you begin your recovery, our physical therapist will advise you to take time during the day to support your arm with your hand elevated above the level of your heart. We will encourage you to move your fingers and thumb occasionally during the day. Keep the dressing on your hand until you return to the surgeon. Avoid getting the stitches wet. Your stitches will probably be removed 10 to 14 days after surgery.
Pain and numbness generally begin to improve after surgery, but you may have tenderness in the area of the incision for several months.
Although each patient recovers at a different rate, you will probably need to attend our occupational or physical therapy sessions for six to eight weeks, and you should expect full recovery to take several months. We will start by having you begin doing active hand movements and range-of-motion exercises. Our physical therapistss also use ice packs, soft-tissue massage, and hands-on stretching to help with your range of motion. When your stitches are removed, we may suggest that you start carefully strengthening your hand by squeezing and stretching special putty.
As you progress, our physical therapist will give you exercises to help strengthen and stabilize the muscles and joints in the hand. We use other exercises to improve fine motor control and dexterity. Some of the exercises you'll do are designed get your hand working in ways that are similar to your work tasks and sport activities.
Our physical therapist will help you find ways to do your tasks that don't put too much stress on your hand and wrist. Before your physical therapy sessions end, your physical therapist will teach you a number of ways to avoid future problems.
When your recovery is well under way, regular visits to Miller PT will end. Although we will continue to be a resource, you will eventually be in charge of doing your exercises as part of an ongoing home program.
Miller PT provides services for physical therapy in Delray Beach.
Physician Review
If it is unclear on physical examination where the nerve is being squeezed, electrical studies may be ordered to try to find the area of compression.
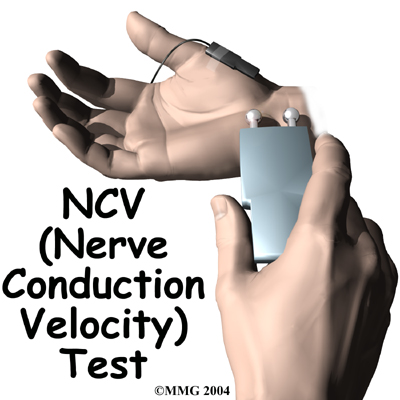 that measures how fast nerve impulses travel along the nerve.
that measures how fast nerve impulses travel along the nerve.
Your doctor might want this test to be done to help pinpoint your problem. Special tests may be required to study the nerve.
The NCV is sometimes combined with an electromyogram (EMG). The EMG is done by testing the muscles of the forearm that are controlled by the ulnar nerve to determine if they are working properly.
If the test shows a problem with the muscle, the nerve that goes to the muscle might not be working correctly.
This is similar to checking whether the wiring in a lamp is working.
If the light still doesn't work after you've put in a new bulb, you can begin to tell if there's a problem in the wiring.
If your symptoms started after a traumatic wrist injury, X-rays may be needed to check for a fractured or dislocated bone.
Surgery
If all attempts to control your symptoms fail, surgery may be suggested to reduce the pressure on the ulnar nerve.
 The surgery can be done using a general anesthetic (one that puts you to sleep) or a regional anesthetic.
The surgery can be done using a general anesthetic (one that puts you to sleep) or a regional anesthetic.
A regional anesthetic blocks the nerves going to only a portion of the body. Injection of medications similar to lidocaine are used to block the nerves for several hours.
This type of anesthesia could be an axillary block (only the arm is asleep) or a wrist block (only the hand is asleep).
The surgery can also be performed by simply injecting lidocaine around the area of the incision.
Once you have anesthesia, your surgeon will make sure the skin of your palm is free of infection by cleaning the skin with a germ-killing solution.
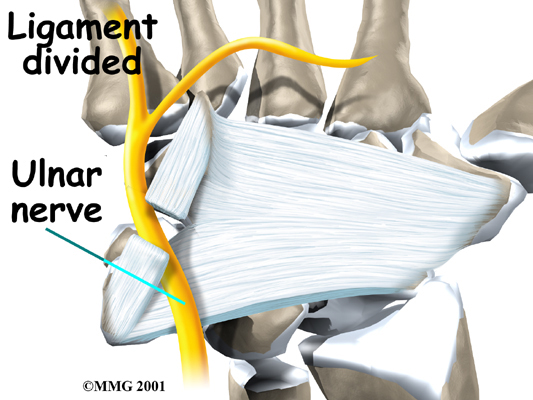
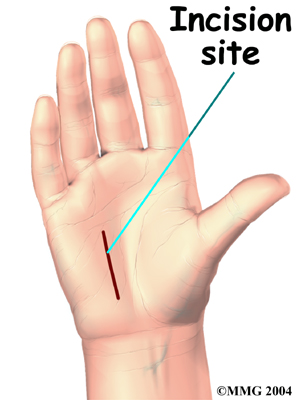
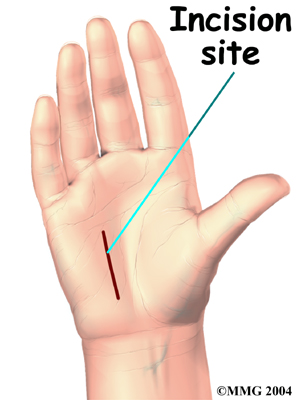
A is made in the palm of the hand over the spot where the nerve goes through the canal.
The incision makes it possible for the surgeon to see the ligament that crosses over the top of the ulnar nerve.
This ligament forms the roof over the top of Guyon's canal.
Once in view, this by using a scalpel or scissors.
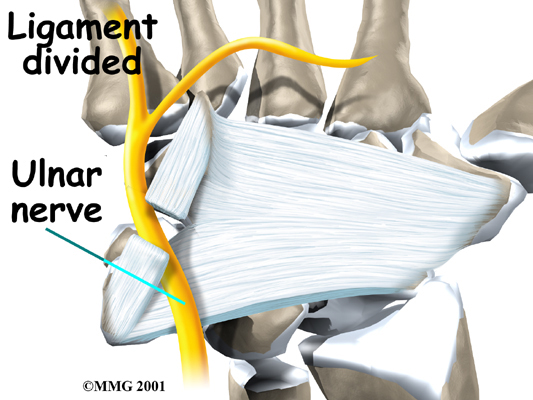
Care is taken to make sure that the ulnar nerve is out of the way and protected. By cutting the ligament, pressure is taken off the ulnar nerve.
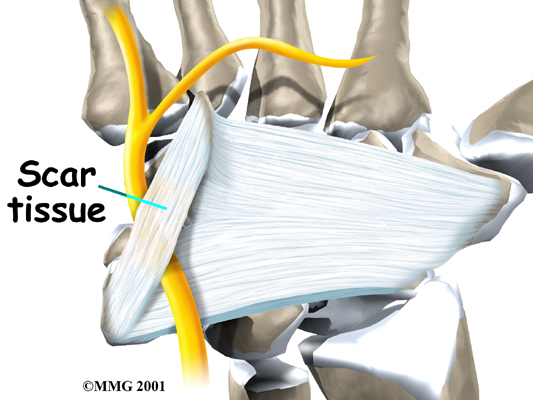
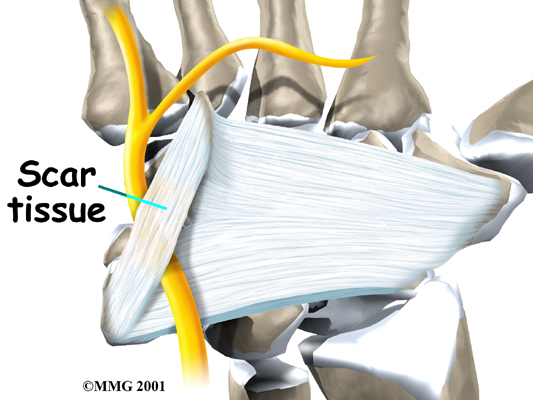
Upon releasing the ligament, the surgeon sutures just the skin together and leaves the loose ends of the ligament separated. The loose ends are left apart to keep pressure off the ulnar nerve. Eventually, the gap between the two ends of the ligament fills in with . This surgery can usually be done as an outpatient procedure, meaning you can leave the hospital the same day.
Portions of this document copyright MMG, LLC.







 Guyon's canal syndrome has several causes. Overuse of the wrist from heavy gripping, twisting, and repeated wrist and hand motions can cause symptoms. Working with the hand bent down and outward can squeeze the nerve inside Guyon's canal.
Guyon's canal syndrome has several causes. Overuse of the wrist from heavy gripping, twisting, and repeated wrist and hand motions can cause symptoms. Working with the hand bent down and outward can squeeze the nerve inside Guyon's canal.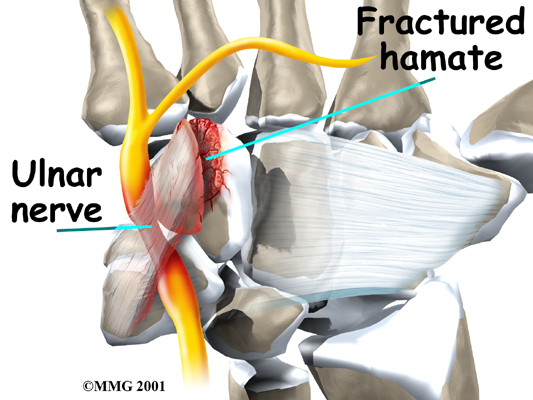
 We may have you wear a
We may have you wear a  Your hand will be wrapped in a
Your hand will be wrapped in a 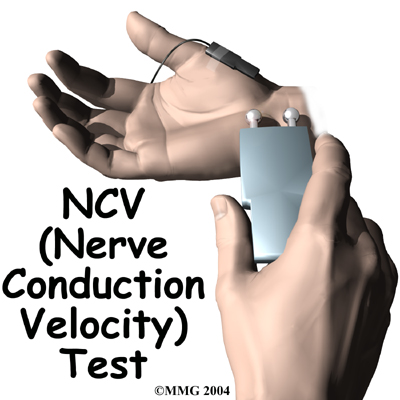
 The surgery can be done using a general anesthetic (one that puts you to sleep) or a regional anesthetic.
The surgery can be done using a general anesthetic (one that puts you to sleep) or a regional anesthetic.